Executive Summary
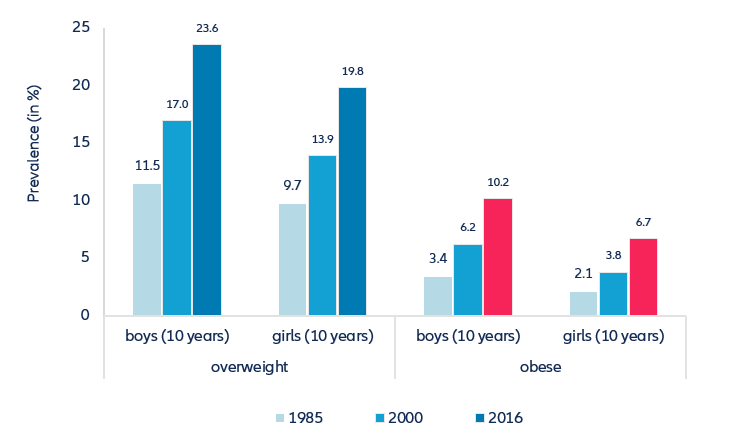
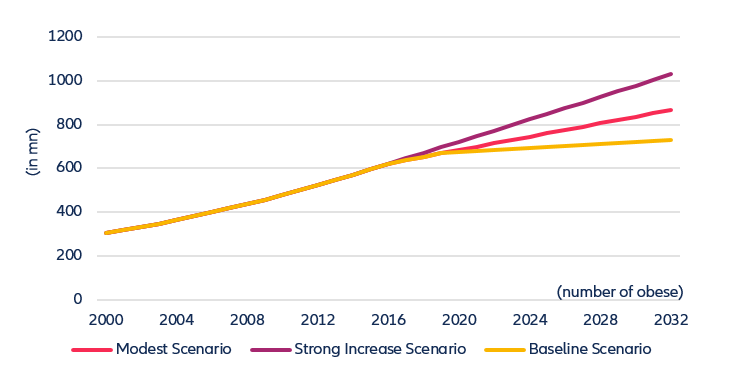
- The share of people who are overweight and obese has been increasing markedly, even in poorer countries, a trend that was likely amplified by the lockdowns imposed during the Covid-19 pandemic. Furthermore, rising prices for fruits and vegetables make a healthy diet unaffordable for an increasing share of the population. In 2032, more than 1bn people worldwide could be obese, up from 650mn in 2016.
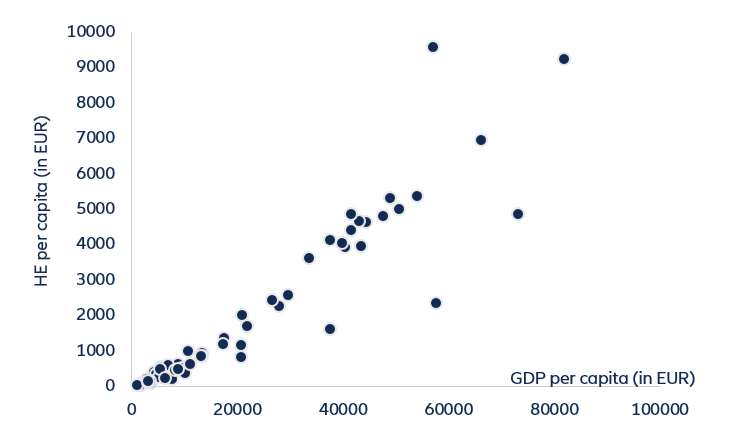
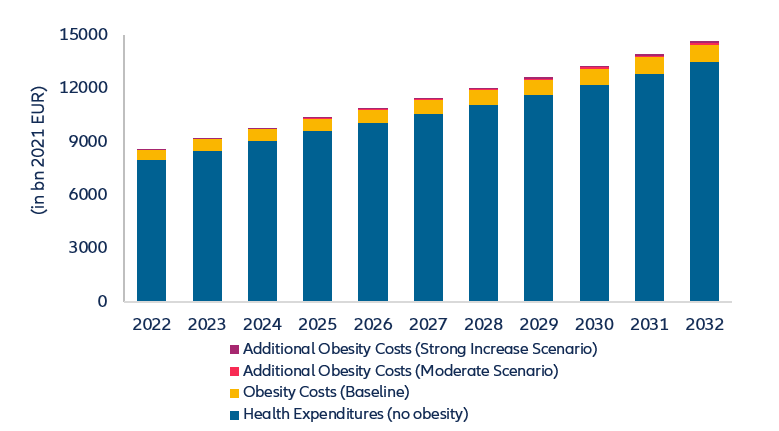
- Obesity already accounts for an estimated 6.8% of total health expenditures as it is a major risk factor for type 2 diabetes, strokes and cardiovascular diseases. Based on our health expenditure projections, we estimate that obesity-related health expenditures could reach EUR1.2trn corresponding to 8.1% of total health expenditures in 2032, driving the accumulated additional health expenditures for the 10-year period up to EUR9.0trn.
- Combined efforts are needed to support healthier lifestyles. The recommendations to achieve this goal range from taxing sugary beverages to the use of health apps, insurance tariffs rewarding a healthy lifestyle and changes in investor behavior, who could take a leaf out of the climate action book, encouraging food producers and processors to disclose their “sugar footprint”, too, with the clear intention to lower it over time.
The unfolding of an epidemic
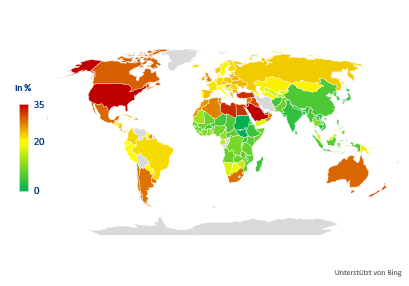
The combination of increasingly sedentary lifestyles and the increased consumption of high-calorie food has led to a rising share of overweight and obese people worldwide. The World Health Organization (WHO) estimates that more than 650mn adults are obese. The differences between and within the regions are, however, very pronounced. In North America, North Africa and the Middle East, as well as in Mexico, Argentina, Australia and New Zealand, between 30% and 40% of the population are obese. In Western Europe, the shares range between 20% and 25%, while in most Asian and African countries they are still below 10% (see Figure 1).
Figure 1: Marked differences in the prevalence of obesity